
My final bike ride through DC
Third-year University of Pittsburgh Doctor of Physical Therapy (DPT) Hybrid student Amanda Klein from Spokane, WA, completed her third of four clinical education experiences over the summer. Klein, a U.S. Air Force veteran, was awarded a special clinical education placement at Walter Reed National Military Medical Center (WRNMMC) in Bethesda, MD, and has been sharing her insight with current and prospective students by writing this short blog series. In her final installment, Klein reflects on this invaluable experience and how it broadened her skillsets and influenced her career goals.
Hello again everyone! Over the summer, I spent 15 weeks at the National Intrepid Center of Excellence (NICoE) adjacent to WRNMMC. At the NICoE, I worked with active-duty service members in a four-week intensive outpatient program for medical management of mild-to-moderate traumatic brain injuries (TBI). I was part of an interdisciplinary care team that addressed the physical and cognitive challenges that occur in patients with TBI. It was an incredible, challenging experience and I’m grateful for the opportunity that I had. I’m back home in Washington state now and currently in my fourth and final clinical education experience. Next stop – graduation!

Washington National Cathedral
How did the clinical at Walter Reed National Military Medical Center add to your DPT educational experience? Did you learn anything beyond what you learned in your classes?
Clinical education experiences are meant to enhance what we learn in didactic lessons in general and my time at WRNMMC was no different. It allowed me to hone my skills and I learned so much more about mild-to-severe TBI than I could have ever learned in a classroom. In class we primarily learned about the physical rehabilitation process, while at NICoE I learned about how art, movement and mindfulness can help people process the mental health and cognitive difficulties that often coincide with TBI.
I also learned so much more about vestibular diagnoses. We spend a lot of time in class learning about benign paroxysmal positional vertigo (BPPV), and with good reason, it’s the most common dizziness disorder in a classic outpatient setting. However, there are so many diagnoses to consider. In 15 weeks I didn’t see a single case of BPPV, but I did see central vestibulopathy, persistent postural perceptual dizziness (PPPD), visual motion intolerance, utricular dysfunction and vestibular migraine – just to name a few. But more importantly I learned that sometimes people who have sustained one or more concussions are just…dizzy, and there’s not a lot that can be done.
School doesn’t always teach you how tough it is when you have no diagnosis other than, “That just happens sometimes, but here’s what we can try.” The vestibular evaluation itself and the assessment and interpretation of the results are much more challenging than we could learn in class. It involves a lot of time taking the patient’s history, knowing what to ask and what pieces make up the puzzle of dizziness for that specific individual. This all takes a lot of clinical-based experience and the reasoning gained from seeing a lot of patients. It’s a skillset I’m lucky to have learned and have used in my new rotation.

The tower building of WRNMMC.
What were your top three highlights working at WRNMMC?
My clinical instructor: she was incredible. She met my needs as a student and really made the experience what it was. Her expertise and ability to teach it in a way that made sense at a beginner level was so beneficial. She was supportive when I messed up or had no clue what was going on. She made me feel confident about my judgment as a clinician and challenged my assessments and interpretations to make me think outside the box. We saw some really cool stuff together and shared a lot of laughs.
The therapy dogs – enough said there, really. Working anywhere with dogs available is incredible. Not only were they cute, but they were also highly trained and it was so fun to watch the providers and the patients interact with them. The dogs were used as therapy devices to help the service members practice mindfulness, patience, memory skills, etc. and the dogs just loved their jobs (and the treats, of course).
The gadgets! I got to see so many incredible tools for testing and rehabilitation that you don’t see much in the “normal” world. I got to experience using VNG (videonystagmography goggles), a Bertec and a Neurocom, and I was able to watch patients undergo treatments in a CAREN (computer assisted rehabilitation environment). These are all incredible tools that can be used for physical and occupational therapy, but aren’t frequently seen outside of specialty places due to the associated price tag. Seeing how these technologies can help people makes me excited for the future of medical technology and how it may translate into the rehabilitation world.
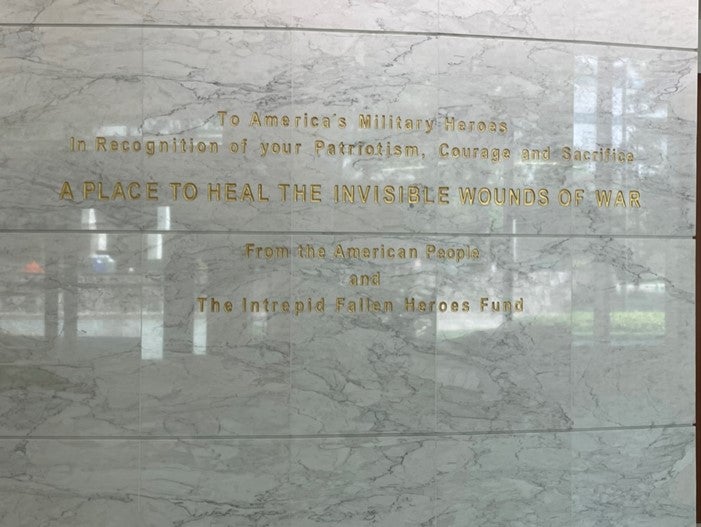
The engraving in the lobby of the NICoE
What was it like working with fellow service-members?
It was so fun to work with the men and women I met over the summer. I love the military community because there is always something you have in common. Many of my patients had been to Alaska (my home state), Washington (my current state) and Okinawa, Japan (my former duty station), so there was plenty to talk about and reminisce over.
Some of the patients I treated knew each other from training, deployments or other duty stations before they ever came through the program and watching them reconnect with old friends added another layer of fun to the mix. It reminded me that, overwhelmingly, the military is a small world that exists in its own bubble. It’s all about “found family,” those in life you meet along the way who become like your own; you can really find anything to connect over and talk about no matter how different you are. Hearing all their crazy stories, sharing mine and finding the other things we had in common is part of what made working at WRNMMC a great experience. There were a lot of laughs. The antics were top tier as usual, but what was more important was connecting over the less fun aspect of the military lifestyle. It’s hard to put into words the understanding that occurs between a vast community of people that just know. I knew them, and they knew me as soon as they found out I’m a vet and that connection was probably the most important.

View of the Spokane River from a local restaurant.
Did the experience influence what you want to do after graduation?
Absolutely it did. So many of the lessons I learned have carried into my final clinical education experience and will stick with me for as long as I’m a clinician. I would love--and plan to--continue working with the military and veteran population. I’d also love to continue working in vestibular rehabilitation because of how challenging it was. I enjoyed the mix of vestibular and orthopedic care; the variety kept me from getting bored.
-----------------------
Written by: Amanda Klein (DPT ’23)
For more information on the DPT program with hybrid and residential options, please see our website or contact an enrollment specialist at enroll@pitt.edu today!
---
Published December 11, 2023
